Last Updated on January 27, 2022 by Heather Hart, ACSM EP, CSCS
The only thing most runners despise more than someone combining the words “5K” and “marathon” together (as in, “Oh my neighbor’s-cousin’s-sister-in-law just ran a 5K marathon!”) is having their training interrupted by illness. There’s never a good time for an athlete to get sick, but the hope is always that they are healthy enough for the illness to be short lived.
Unfortunately, we are finding that runners who contract any of the COVID-19 (SARS-CoV-2) virus variants are struggling with physically returning to running, struggling to understand the appropriate way to approach their return to running after COVID, and sometimes, both.
There is still so much unknown about this virus and how it affects even healthy individuals, which can absolutely leave runners with hesitation to get back to doing what they love.
This post will discuss:
- How COVID affects a runner’s body, & what can happen if the process of returning to running after COVID is rushed.
- How to know when it’s appropriate to return to running, for both symptomatic and asymptomatic COVID positive runners.
- Recommended return to running and training strategy.
- What signs and symptoms to look for when running to ensure you are not risking your health.
- What Long-COVID runners need to know about running and training.
Foreword and Disclaimer:
March of 2020 seems like only yesterday. At the time, the blogging world came to a screeching halt for a number of reasons, and regardless of niche, we were warned to not talk about COVID. There was an air of “taboo” surrounding the subject: so much was unknown and controversial, and apparently, the entities that determine things such as search engine page rank frowned upon mentioning this pandemic (we were also urged to not mention the word “pandemic”. But I did write this post about running indoor ultras that I’m still pretty proud of. )
But here we are nearly two years later. COVID 19 has presented us with a number of variants, and has affected people of all walks of life in different ways. As a full time running coach, I have seen dozens of clients through COVID diagnosis, and helped them make their return to regular training.
Further, as I sit here now, I am 12 days post onset of symptoms, and 6 days post official COVID diagnosis, and about to navigate the whole “when should I start running again” scenario myself.
Point being: not talking about the elephant in the room seems like it’s no longer an option. So, whether it’s a smart move or not, I’m writing this post. Please note, I am an ACSM certified Exercise Physiologist as well as a certified running coach through a number of organizations. However, I am not a doctor, and I am not a specialist when it comes to returning to physical activity post COVID. I am presenting information that has been presented to me from actual experts in this field, as well as passing on a number of other citations in the field.
PLEASE CONSULT YOUR PHYSICIAN if you have any questions or concerns regarding returning to running after COVID 19, or if you are struggling with training while experiencing long COVID symptoms.
How COVID is Affecting Runners:
It’s important to emphasize that this virus has been shown to be physically detrimental to the human body in a number of ways that far extend beyond the “lung issues” that were initially focused upon early in 2020.
So far, research as discovered more than 50 different long term effects from COVID-19 infections (7)
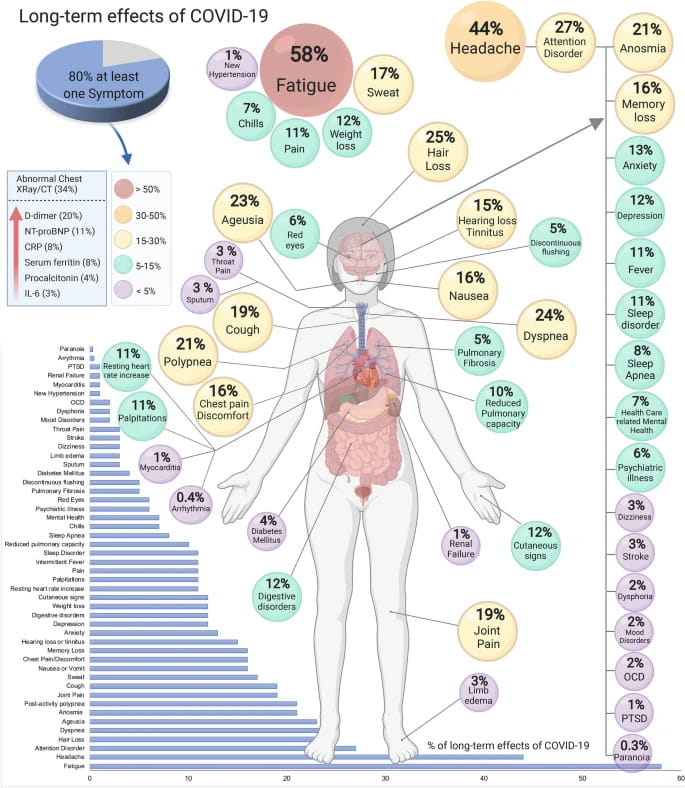
And the symptoms aren’t only presenting themselves during the initial sickness. A systemic review and meta-analysis of 47,910 patients who tested positive for COVID determined that 80% of those patients developed one or more long-term symptoms (upwards of 110 days post-viral infection). The five most common symptoms were fatigue (58%), headache (44%), attention disorder (27%), hair loss (25%), and dyspnea (24%). (7)
Researchers still aren’t entirely sure why the virus has caused such a variety of symptoms, and why it has been so damaging in many cases. But they are emphasizing the importance of being cautious when it comes to returning to exercise, such as running, after experiencing COVID.
Here are some of the specifics as to why:
Immune System Response:
When your body becomes infected with a virus like COVID, your immune system springs to action. It utilizes a slew of white blood cells – such as macrophages, B-cells, and T-cells – to identify, mark, destroy, and get rid of the virus in your body.
Cytokines are a type of protein used as a chemical messenger between all of the different types of cells that make up your immune system, so they can coordinate their attack. But, cytokines are also responsible for triggering things like fever, aches, chills, inflammation, runny nose, and other symptoms commonly associated with viruses.
Aerobic exercise – such as running – is known to cause an acute immune system inflammatory response, even in healthy individuals (3). Typically this is a good thing, as an acute reaction helps make your immune system stronger.
Related post: Ultramarathons, Immune Systems, and Why You Get Sick After Ultramarathons
Too much of a good thing?
But…too much exercise can have a negative effect on your immune system. Research also shows that exercise of longer duration (greater than 2 hours) and/or harder intensities (greater than >80% of VO2max) is associated with markers of immunosuppression such as:
- increased production of proinflammatory cytokines
- an increase in lower respiratory tract infections
- reduced activity of NK cells, T and B lymphocytes, and macrophages. (6)
The Dreaded Cytokine Storm:
Now, a COVID-19 infection has been shown to sometimes be accompanied by an aggressive inflammatory response with the release of a large amount of proinflammatory cytokines in an event known as “cytokine storm.” (9) That “storm” occurs when your body decides to produce more immune cells, and in turn these new cells release even more pro-inflammatory cytokines.
Excessive cytokine production causes an immune response that can damage organs, especially the lungs and kidneys, and even lead to death. Several studies suggest that the cytokine storm correlated directly with lung injury, multi-organ failure, and unfavorable prognosis of severe COVID-19.
Cardiac Complications
We’ve probably all heard it before: in some cases COVID is affecting the hearts of both athletes and non athletes alike. Various reported cardiac complications from COVID include:
- Arrhythmia: improper beating of the heart, whether irregular, too fast, or too slow, due to electrical impulses that are not working properly. Symptoms may include a fluttering in the chest, chest pain, fainting, or dizziness.
- Myocarditis: inflammation of the heart muscle tissue. In severe cases, myocarditis can weaken the heart, which can lead to heart failure, abnormal heartbeat, and sudden death. Symptoms include chest pain, abnormal heartbeat, and shortness of breath.
- Acute myocardial injury: where at least one cardiac troponin (cTn) concentration is above the 99th percentile upper reference limit . Troponin is a type of protein found in the muscles of your heart, that is only released into the blood stream when the heart muscle has sustained damage.
Why You Shouldn’t Rush to Get Back to Training:
A lot is still woefully unknown when it comes to our bodies responses to a COVID infection. Because of that, experts are recommending that athletes and general fitness seekers do not rush to return to physical activity. Not only may the exertion put additional stress upon your body, and potentially increase the risk of increased inflammation and risk of respiratory infection, but you may also be putting your heart at risk.
Authors of the scientific review article “Considerations for Return to Exercise Following Mild-to-Moderate COVID-19 in the Recreational Athlete” state the following:
“While regular exercise improves cardiovascular health in the long-term, each session of exercise stresses the heart and can trigger potentially lethal arrhythmias in the context of underlying cardiovascular disease. Many nonhospitalized individuals with COVID-19 will likely not develop cardiac manifestations and be able to safely return to exercise. Despite this, care must be taken to ensure the absence of persistent cardiac complications related to COVID-19 prior to returning to exercise. (8)“
What if I’m Asymptomatic?
In much of what scientists still don’t understand, is why some individuals infected with the SARS-CoV-2 virus are either showing minimal symptoms, or are completely asymptomatic.
If that’s the case, and you otherwise “feel” fine, can you still run?
Experts are saying it’s not worth the risk. According to a January 24th, 2022 published update from the American College of Cardiology Sports & Exercise Leadership Council asymptomatic athletes with COVID-19, are recommend to abstain from exercise for three days to ensure that symptoms do not develop. For athletes with non-cardiopulmonary symptoms, exercise training should generally be withheld until symptom resolution.
Returning To Running After COVID: When to Start & How to Safely Approach Training
After reading all of the above, you may find yourself feeling a little hesitant to return to running. No one can blame you there. But it’s important to remember the following:
- Statistics show that consistently meeting physical activity guidelines was strongly associated with a reduced risk for severe COVID-19 outcomes among infected adults. (10)
- Further, initial studies show that there may be a relationship between maximal aerobic capacity (VO2 max) and the severity of COVID symptoms. Those with a higher VO2 max were less likely to be hospitalized than those who were less fit. (1)
- Physical activity is associated with positive mental health.
The benefits of regular physical activity cannot be denied. Many of the scary, but very real, complications mentioned above are rare. It’s incredibly important to be aware of them, and do everything you can to help prevent them from happening. But ultimately, moving your body will help keep you healthy. So please don’t be afraid to get back at it.
Related Post: Trail Running’s Effect on Mental Health – 5 Proven Ways Trail Running Makes You Happy
Should I See My Doctor Before Returning to Running?
Wondering if you should see a doctor before attempting to hop back into your training cycle? In my professional opinion, if you are wondering at all, the answer is yes, yes you should see your doctor to ensure that there are no lasting concerns before returning to running.
More specifically, in the article: “Cardiorespiratory considerations for return-to-play in elite athletes after COVID-19 infection: a practical guide for sport and exercise medicine physicians”, researchers recommend the following:
No formal respiratory testing is required for runners who:
- Were without symptoms or signs of COVID-19 during the pandemic
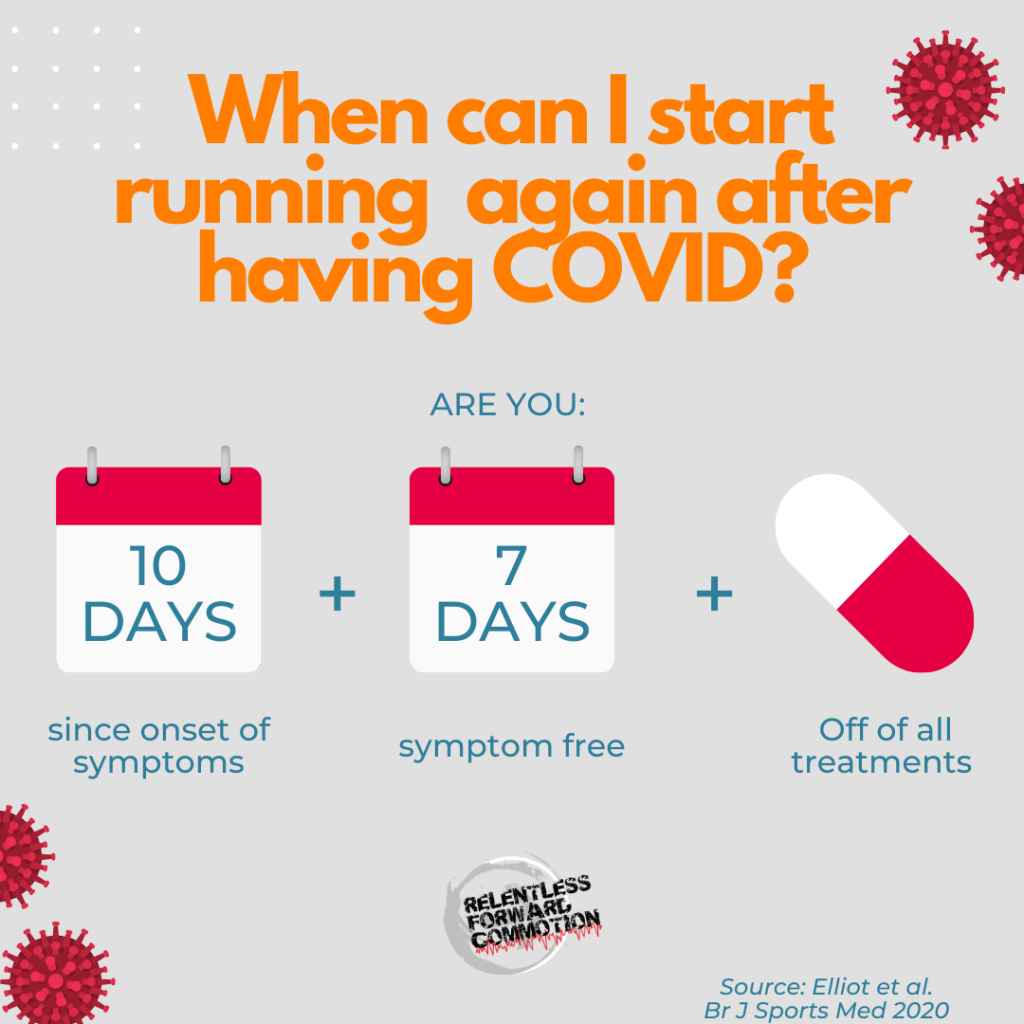
- Athletes with mild to moderate COVID-19 symptoms who managed their condition at home but are now fully recovered (symptom free at rest for 7 days and no sooner than day 10 from the onset of symptoms) (12)
Researchers note that even in this category, a deviation from your normal running experience (i.e. if symptoms do start to show up) requires a visit to your doctor.
Consult your doctor before returning to running if:
- You have documented underlying respiratory issues, such as asthma.
- COVID-19 related respiratory symptoms that are persistent and taking longer than 14 days to recover.
- You have experienced respiratory symptoms or other COVID related symptoms severe enough to require hospital admission.
- You have any questions, concerns, or hesitations at all.
What Sort of Tests Should I Ask My Doctor For?
Recommended tests to have before returning to running include:
- Electrocardiogram (ECG/EKG -they are the same thing)
- Blood tests, specifically looking for troponin, a marker of heart injury
- Chest x-ray
Post COVID Timeline:
According to experts, you’ll want to consider the following before gradually returning to running after COVID:
- You should have at least 10 days out from the onset of COVID symptoms, 7 days symptom-free, and off of all COVID related treatments before returning to exercise.
- You should be able to complete activities of daily living (dressing yourself, showering, household chores, etc.) and walk 500 m on a flat surface, without excessive fatigue or breathlessness. (5)
Some additional monitoring may add value to understanding how well your body is recovering. Consider your:
- Resting heart rate – is it still significantly elevated, or closer to normal values? If elevated, this may be a sign that your body is still fighting off infection, and you should continue resting.
- Rate of perceived exertion – if normal activities or what you would normally consider “easy” exercise (such as a warm up) feels incredibly difficult, you may want to continue resting.
- Sleep, stress, fatigue and muscle soreness – listen to cues from your body to see if it is still working hard, or if it is rested and ready to train again.
- Injury-Psychological Readiness to Return to Sport – How do you mentally feel about returning to running? If you’re concerned or hesitant – wait.
Researchers note that some athletes take well over 3 weeks to recover, with more intense sports (such as running) sometimes taking a longer recovery period before returning.
The Graduated Return Protocol
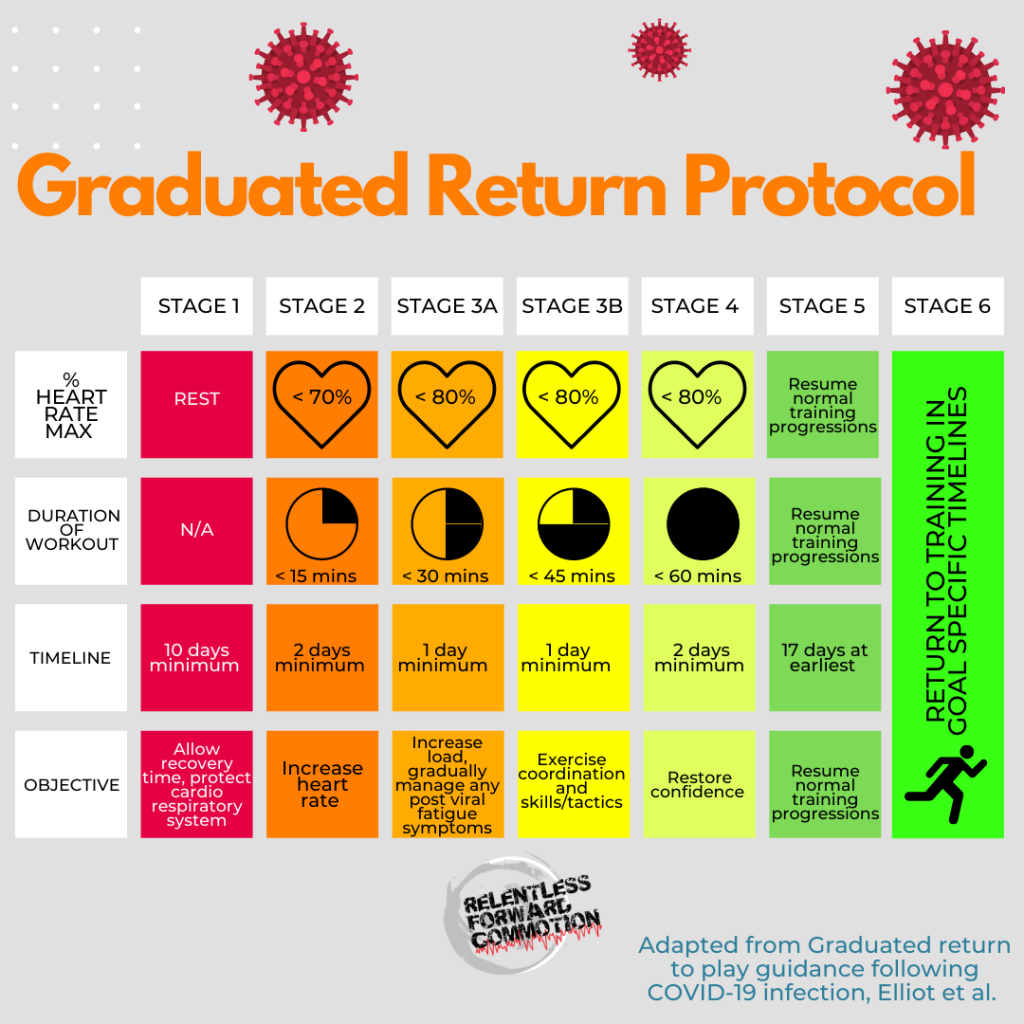
The Graduated Return Protocol, or GRTP, is a stepping stone process to help you return to physical activity or running, recommended by the English Institute of Sport, Sportscotland Institute of Sport, & others.
This protocol is a 7 day process that can begin as soon as 10 days post onset of symptoms, as long as the runner is cleared for exercise.
- Stage 1: The first stage covers the minimum 10 days rest recommended.
- Stage 2: A maximum of 15 minutes of exercise, at a heart rate no greater than 70% of your maximum heart rate. This stage should be repeated for two days.
- Stage 3A: A maximum of 30 minutes of exercise, at a heart rate no greater than 80% of your maximum heart rate. This stage should be repeated for one day.
- Stage 3B: A maximum of 45 minutes of exercise, at a heart rate no greater than 80% of your maximum heart rate. This stage should be repeated for one day.
- Stage 4: A maximum of 60 minutes of exercise, at a heart rate no greater than 80% of your maximum heart rate. This stage should be repeated for two days.
- Stage 5: At no sooner than 17 days post onset of COVID symptoms, you may resume normal activity if you’ve reached stage 5 without incident.
- Stage 6: Return to normal training, whatever that may be for you (marathon training plan? Ultramarathon training cycle? etc.)
NOTE: If any symptoms occur (including excessive fatigue) while going through GRTP, experts recommend returning to the previous stage and progressing again after a minimum of 24 hours period of rest without symptoms.
The 50/30/20/10 Protocol
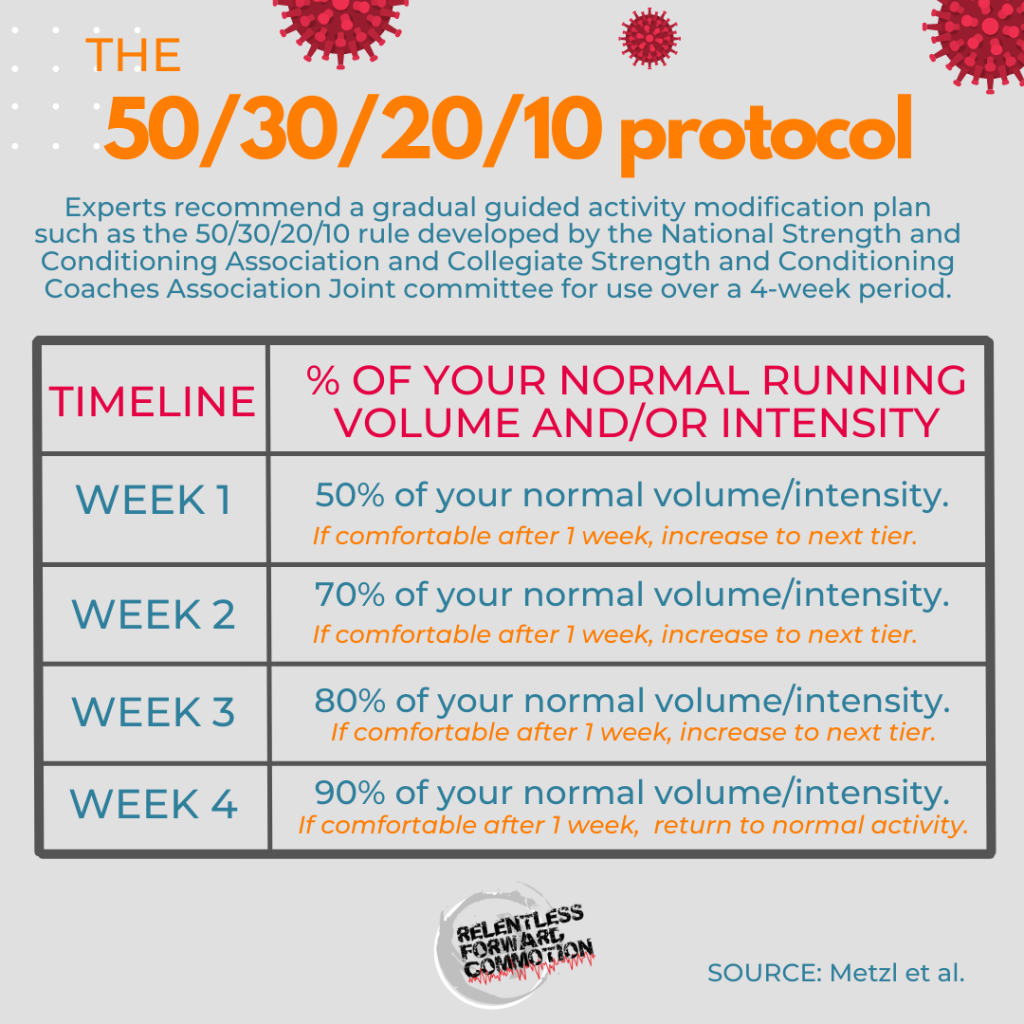
In “Considerations for Return to Exercise Following Mild-to-Moderate COVID-19 in the Recreational Athlete”, researchers recommend a gradual guided activity modification plan such as the 50/30/20/10 rule developed by the National Strength and Conditioning Association and Collegiate Strength and Conditioning Coaches Association Joint committee for use over a 4-week period.
In this protocol, running volume for the first week is reduced by at least 50% of your normal volume, followed by 30%, 20%, and 10% in the following 3 weeks if comfortable at the end of each week. For example:
- Week one: run 50% of your normal running volume.
- Week two: run 70% of your normal running volume.
- Week three: run 80% of your normal running volume.
- Week four: run 90% of your normal running volume.
- Week five: return to your normal running volume.
Similar to the GRT protocol, if any symptoms occur, or if you are struggling to maintain the volume for a given week, you should return to the previous stage and progressing again after you feel more comfortable with the load.
Signs & Symptoms to Be Aware of:
When returning to running after COVID, it’s important to be aware of symptoms that may indicate something isn’t quite right. If you experience any of the following, stop running immediately and follow up with your doctor:
- chest tightness or pain
- excessive shortness of breath or feeling winded, beyond what is normal for you in running at a given effort
- feeling lightheaded or passing out
- excessive fatigue
- features of thrombosis, such as a swollen calf, tachycardia (a rapid or irregular heartbeat that doesn’t correlate to your activity), or breathlessness.
Again, it’s important to remember that there is a lot that is still unknown about how our bodies are responding to COVID-19 infections. Therefore, if you experience any new, unpleasant or questionable symptoms when returning to running after COVID, besides what is already listed above, consult your physician.
Long COVID & Running: What You Need to Know
According to the CDC, Long COVID, also referred to as long-haul COVID, Post-COVID Syndrome, and a slew of other terms, refers to the wide range of physical and mental health consequences experienced by some patients that are present for 4 or more weeks after a COVID infection. This includes patients who may have had mild symptoms, or were even asymptomatic during infection. Here are some things to keep in mind:
- A study of patients with Long COVID published in the June 2021 Fair Health White Paper showed that 23.2% of 1,959,982 COVID-19 patients had at least one or more symptoms of COVID 30 days after their initial diagnosis.
- Another study of 3,762 respondents in 53 countries with Long COVID (lasting longer than 28 days) found that 89.1% experienced post-exertional malaise, or worsening/relapse of symptoms after physical or mental activity. (4)
What does this all mean?
This data demonstrates that not everyone is responding to, nor recovering from, COVID-19 infections the same. Therefore, it’s incredibly important to remember that there is no one-size-fits-all recovery timeline, and that when attempting to return to running after COVID, you remain patient.
Final Thoughts:
Listen, none of us want to be here. Nearly two years ago we all imagined this would be done and over with in our 15 day initial quarantine. But as for now, it appears that COVID-19 is not going away anytime soon, and has become something that endless runners have had to deal with – and endless runners likely will have to deal with in the future.
My advice?
If you are recovering from COVID and anxious to get back to training, I encourage you to listen to your body. Prioritize sleep, and reduce stress as best as possible. Nourish and hydrate your body in a way that helps promote a healthy, happy immune system. And most importantly, do not rush your return.
Know that in many cases, the return to feeling “normal” during physical activity is seemingly much longer than that of a standard cold or the flu. Be patient and forgiving to your body while it continues to heal from COVID, no matter how bad your symptoms were.
You will thank yourself in the long run (pun always intended).
Resources:
- Brawner, C. A., Ehrman, J. K., Bole, S., Kerrigan, D. J., Parikh, S. S., Lewis, B. K., Gindi, R. M., Keteyian, C., Abdul-Nour, K., & Keteyian, S. J. (2021). Inverse Relationship of Maximal Exercise Capacity to Hospitalization Secondary to Coronavirus Disease 2019. Mayo Clinic proceedings, 96(1), 32–39. https://doi.org/10.1016/j.mayocp.2020.10.003
- Cappanera, S., Palumbo, M., Kwan, S. H., Priante, G., Martella, L. A., Saraca, L. M., Sicari, F., Vernelli, C., Di Giuli, C., Andreani, P., Mariottini, A., Francucci, M., Sensi, E., Costantini, M., Bruzzone, P., D’Andrea, V., Gioia, S., Cirocchi, R., & Tiri, B. (2021). When Does the Cytokine Storm Begin in COVID-19 Patients? A Quick Score to Recognize It. Journal of clinical medicine, 10(2), 297.
- Cerqueira, É., Marinho, D. A., Neiva, H. P., & Lourenço, O. (2020). Inflammatory Effects of High and Moderate Intensity Exercise-A Systematic Review. Frontiers in physiology, 10, 1550. https://doi.org/10.3389/fphys.2019.01550https://doi.org/10.3390/jcm10020297
- Davis, H. E., Assaf, G. S., McCorkell, L., Wei, H., Low, R. J., Re’em, Y., Redfield, S., Austin, J. P., & Akrami, A. (2021). Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine, 38, 101019. https://doi.org/10.1016/j.eclinm.2021.101019
- Elliott, N., Martin, R., Heron, N., Elliott, J., Grimstead, D., & Biswas, A. (2020). Infographic. Graduated return to play guidance following COVID-19 infection. British journal of sports medicine, 54(19), 1174–1175. https://doi.org/10.1136/bjsports-2020-102637
- Leandro, C. G., Ferreira E Silva, W. T., & Lima-Silva, A. E. (2020). Covid-19 and Exercise-Induced Immunomodulation. Neuroimmunomodulation, 27(1), 75–78. https://doi.org/10.1159/000508951
- Lopez-Leon, S., Wegman-Ostrosky, T., Perelman, C. et al. More than 50 long-term effects of COVID-19: a systematic review and meta-analysis. Sci Rep 11, 16144 (2021). https://doi.org/10.1038/s41598-021-95565-8
- Metzl, J.D., McElheny, K., Robinson, J.N. et al. Considerations for Return to Exercise Following Mild-to-Moderate COVID-19 in the Recreational Athlete. HSS Jrnl 16, 102–107 (2020). https://doi.org/10.1007/s11420-020-09777-1
- Ragab, D., Salah Eldin, H., Taeimah, M., Khattab, R., & Salem, R. (2020). The COVID-19 Cytokine Storm; What We Know So Far. Frontiers in immunology, 11, 1446. https://doi.org/10.3389/fimmu.2020.01446
- Sallis, R., Young, D. R., Tartof, S. Y., Sallis, J. F., Sall, J., Li, Q., Smith, G. N., & Cohen, D. A. (2021). Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: a study in 48 440 adult patients. British journal of sports medicine, 55(19), 1099–1105. https://doi.org/10.1136/bjsports-2021-104080
- Scheffer, D., & Latini, A. (2020). Exercise-induced immune system response: Anti-inflammatory status on peripheral and central organs. Biochimica et biophysica acta. Molecular basis of disease, 1866(10), 165823. https://doi.org/10.1016/j.bbadis.2020.165823
- Wilson, M. G., Hull, J. H., Rogers, J., Pollock, N., Dodd, M., Haines, J., Harris, S., Loosemore, M., Malhotra, A., Pieles, G., Shah, A., Taylor, L., Vyas, A., Haddad, F. S., & Sharma, S. (2020). Cardiorespiratory considerations for return-to-play in elite athletes after COVID-19 infection: a practical guide for sport and exercise medicine physicians. British journal of sports medicine, 54(19), 1157–1161. https://doi.org/10.1136/bjsports-2020-102710
Heather Hart is an ACSM certified Exercise Physiologist, NSCA Certified Strength and Conditioning Specialist (CSCS), UESCA certified Ultrarunning Coach, RRCA certified Running Coach, co-founder of Hart Strength and Endurance Coaching, and creator of this site, Relentless Forward Commotion. She is a mom of two teen boys, and has been running and racing distances of 5K to 100+ miles for over a decade. Heather has been writing and encouraging others to find a love for fitness and movement since 2009.



Becky Ryder
I am a 77 year old female runner for nearly 55 years. I am 11 days out from positive test with relatively mild symptoms, with the exception of fatigue and muscle soreness. I needed a slap in the face to make me realize I need to be cautious and patient as I attempt to return to running. Thanks for all the information and much needed advice.
Kevin
Thanks for this useful piece, based on experience and research. Here I am, a seasoned half-marathoner on day 7 of covid and feeling over the worst and wondering when I should lace my trainers again, having missed my first race of the season this weekend…the answer? Stop being foolish and wait ! I will of course…I think the dog will wonder why so many walks once I am symptom free!
Jody
I’m at Day 7 of COVID, still managing my headache with Motrin but trying to gauge for when I can start working out again. Remembered this article I read a year ago and came back to it. Thank you so much for this well-written easy to read article. (COVID brain is still real for me). I’ll refencing this in the next couple of weeks to remind myself to take it slow.
Heather Hart, ACSM EP, CSCS
I hope you feel better soon, Jody!